Learning the Lessons of Back Painthe Hard Way
On that bitter day, I understood why some people have the morning paper delivered to their door. That early morning, despite the warnings from my wife about the slippery slippers, I donned those evil Totes and fetched the paper from the end of the driveway. On my return, I slipped and fell at an obscene angle landing in an angled (mangled?) position on my butt. The loud pop suggested something very bad just occurred in my lumbar area. In retrospect, I do not think that this was the primary cause of my back problem, but rather, the straw that broke the camel’s back. First Lesson: Always listen to your wife when she is trying to help you. Use your common sense when it comes to icy New England winters! And why do you think they call them slippers? In the weeks that followed, I felt stiffness in my lower back, and clicking in my lower back upon waking in the morning, like the joint was loose (like a knuckle crack). At this time, I was still employed and traveled on business. A trip in April to the west coast almost killed me, as the pain in the middle and lower back was unbearable. Sitting became almost impossible. My overall energy level drastically decreased and I felt normal energy levels in the morning, but the rest of the day felt exhausted. My entire lower back was uncomfortable, tight, and abnormal. In May of 2003, performing my duties at work was getting difficult. I notified HR that my condition was noticeably affecting my overall well-being, as well as ability to commit to hours more than 40 hours per week. No action was taken at that time relative to exploring alternative options. At this time, I started to realize my physical limitations because of my discomfort. I refrained from driving for more than 20-minute periods, or sitting more than 25-30 minutes in any chair. I started to check my blood pressure regularly, and noticed that my blood pressure was above borderline,averaging 150/95. However, I pressed on at work despite the psychological and physical pain. I worked until the stress and high blood pressure rose to the boiling point and I left my full-time job in October of 2003. Second Lesson: Being in chronic pain and doing your best work are usually incompatible. Know when to call it quits to preserve your health, sanity and reputation. Based on a colleague’s recommendation, I consulted a chiropractor and physical therapist. The initial consultation confirmed and localized problem areas. I inquired about the issue of not having X-rays or diagnostics; the chiropractor stated it was not necessary. This did not feel right to me, as I still did not know the exact cause of my condition. I gradually realized that the driving time from between work and the treatment location was too far; sometimes 40-50 minutes, and the sitting in the car was inflaming my condition. Some of the exercises prescribed were uncomfortable to perform particularly sit-ups. On several occasions, I felt and heard “pops” in my tailbone area while doing sit-ups on an exercise ball. To me, sit-ups did not seem to be the right therapy! Third Lesson: Listen to you body and your common sense! If you are being treated without the benefit of a diagnosis — and an understanding of your diagnosis — you may be making your situation worse. The first step in attaining wellness is receiving an accurate diagnosis! In June 2003, I started talking to people (somewhat discretely) about my problem; several people explained their familiarity with tailbone injuries. During this same period, I incorrectly self-diagnosed my condition as a tailbone injury. I then purchased a doughnut cushion, limited my driving, sitting, and finally considered swimming. I also set up a standing station at work. I found this work position tiring, but I was so desperate I stuck with it. My general energy level was considerably below normal (50-60% of healthy levels). In July, I had medical diagnostics performed at Lahey. The spine surgeon indicated that I had degenerative disc disease at L5-S1 and suggested physical therapy, while also suggesting surgical options as a last resort. I inquired further about othe options, including artificial disc replacement, and he suggested that the technology was unproven but promising. He asked me if I really wanted to be a guinea pig, so I immediately discounted artificial disc replacement as a viable solution. Fourth Lesson: Listen to your doctor, but keep an open mind. A doctor may care about your health problem, but his training and business interests may not always guarantee you the best treatment. Like professionals, a doctor’s training and — bag of tricks– may limit the advice that leads to your best health remedy. In August, It became extremely difficult to focus on work, as I was lucid just a few hours a day and uncomfortable almost all of it. My blood pressure was running high, so I switched NSAIDs. Taking naproxen sodium helped initially, but the discomfort continued, so I doubled the dosage. Eventually, stomach discomfort and fatigue forced me to stop. I started taking Vioxx that helped relieve the discomfort considerably; but it raised my blood pressure, while also causing chest pains. It also made me feel very tired! In August of 2003, I gave up doing normal things like eating at restaurants or driving to friends or relatives’ houses. I started swimming, which made me feel better while also lowering my BP. However, most nights after dinner, I started laying down next to the dinner table to finish dinner conversation with my wife, as I could not comfortably sit. It was still difficult to focus and work even 30 hours per week. Feeling frustrated with the lack of proper treatment from my doctor, I selected a new primary care physician. I started physical therapy and attended twice weekly, and traction (applied with a harness) offered the most relief of lower back symptoms. In addition, I started swimming five to six times a week for 20-30 minutes. This regime of physical therapy, NSAIDs and swimming held me at an uncomfortable but manageable plateau for almost eight months. In April 2004, there were gaps in the physical therapy treatments, which I augmented with visits to an inversion (traction) table. Treatments provided immediate relief of lumbar tension and pain, but may have also added to the inflammation in the L5-S1 area. It may have also stretched out my knee joints to the point of audible clicking. In May, I started taking Celebrex, which helped reduce the pain in the lumbar and groin area. Strangely, I felt the hyper-mobility in the lumbar joint return, suggesting that the severe inflammation in L5-S1 was so severe from traction (and dysfunction) that is was constricting movement. Because the inflammation was reduced from Celebrex, the joint was free to move (for better or for worse). My energy returned and my groin pain disappeared. Fifth Lesson: Just because the treatment (in this case, traction) may feel good, it does not mean it is good for you. In fact, it may be causing you harm. During thep lateau period, I continued swimming as often as every day. I taught myself the crawl stroke and was happy to see reduction in both my weight and blood pressure. Unfortunately, I stopped in mid June 2004 because of severe tendonitis in my left shoulder. Sixth Lesson: For people that have spinal problems, swimming can be a double-edged sword. It helps the cardiovascular system, while maintaining flexibility and overall well-being. However, the twisting action of a crawl may not be ideal for a dysfunctional spine! In the winter, I spent hundreds of hours doing online research on lumbar fusion and artificial disc replacement . It was exceedingly difficult finding a comfortable way to work on the computer, so I was forced to lie in an awkward position. I alternated between standing and laying positions for five months; but I paid off as I found a great deal of useful information from online journals and especially from patient communities. Many of the personal reports I read from patients regarding their fusions were downright negative. The first thing I learned is that fusion process can be certainly effective; but the patient’s pain may or may not be alleviated. In addition, there are long-term effects of fusion to consider (premature degeneration in adjacent discs and connective tissues, called Transition Syndrome). I then explored the many risks of lumbar fusion, canceled my scheduled anterior lumbar interbody fusion and focused on learning about artificial disc replacement. Seventh Lesson: Just because fusions have been performed for the past fifty years, it does not mean that they offer the most effective treatment for a spine disorder. And this lesson was made abundantly clear by communicating directly with many fusion patients! Many cold winter months went by while I continued my online research. I began to seriously consider artificial disc replacement as the best possible remedy, while also learning of the many challenges associated with a relatively new medical procedure for American surgeons. Since artificial disc replacement had only been practiced in the U.S. since 2001, the FDA had not yet approved it, thereby limiting insurance coverage of most insurance carriers.
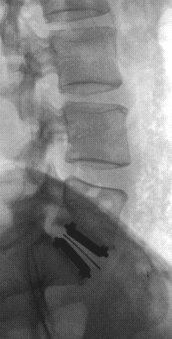
Meanwhile, many people were flying to Europe to have artificial disc replacement , where some surgeons have been honing their artificial disc replacement skills since 1987. Many of these European surgeons were highly sought out for their expertise, low complication rates and good patient outcomes; a few performed over 1000 procedures. Other patients, like me, decided to participate in FDA trials in the United States. After I met with my surgeon, I was impressed with his highly consultative manner, spinal expertise and caring disposition so I opted for the “local” option and had surgery in Boston on June 24th, 2004. My procedure lasted three hours, a bit longer than the average operation time. But the placement of the device was “perfect” and my stay in the hospital was only two days. As I had no pain and very little discomfort, I did not require any painkillers whatsoever after discharge. Eighth Lesson: Do not lose hope if your insurance company will not provide medical coverage for a medical procedure, or if you cannot fly to Europe to see the most “experienced” surgeons. You may have to petition and plead your case with your insurance company for coverage, but do not let it prevent you from attaining the best medical solution. And yes, highly competent and caring surgeons are found in the United States! Take the time to network, ask questions and find a doctor you respect and trust. Since walking is an important aspect of any artificial disc replacement patient’s recovery, I knew that I should get my foot and knee problem diagnosed and treated. So just a few weeks after surgery, I started physical therapy. Surprisingly, the therapist moved me directly into a back rehabilitation program. When I politely and assertively questioned the aggressive nature of the prescribed exercises, he simply sidestepped the issue and continued. The clicking in my tlower back area was not comforting either, as I had no idea what it was or what it might mean down the road. In the second week of therapy, I was performing more aggressive exercises, like torso rotations and even hamstring stretches with dumbbells. I paid for it dearly, as I tore muscles in my still tender abdominal area. My hamstrings were very sore the next day, and two days later the muscles spasms in my left leg hamstring kept me up most of the night. A week later, I was still sore and felt related hamstring problems! I finally spoke with my doctor and we both agreed to terminate the physical therapy program. Ninth Lesson: Artificial disc replacement patients wait at least six weeks to start any physical therapy program. If you even suspect a treatment is not right for you — stop it before you do something detrimental to your recovery! At this writing, six weeks after surgery, I am a new man: full of energy, life and gratitude. I wake with more energy every day, and feel the best I have felt in decades. I plan to return to work soon as a marketing professional while pursuing interests and hobbies that were lost during my dark days of back pain. Recently, and rather unexpectedly, I received a notification from my insurance company that my artificial disc replacement procedure was approved; suggesting I will be reimbursed for the costs of the surgery. Tenth Lesson: Miracles do happen to ordinary people like you and me!!! |